
Cervicogenic Dizziness
by Kaela Pauly, DPT
of Cascade Dizziness & Balance Physical Therapy
(Presented to Seattle Dizzy Group on 4/13/19)
This presentation gives an overview of cervicogenic dizziness including common causes (such as neck, head, or brain injury), signs and symptoms, and how physical therapy can help.
What Is Cervicogenic Dizziness?
Cervicogenic Dizziness (CD) is dizziness associated with neck dysfunction and/or pain caused by direct injury to the neck. To understand CD, a basic understanding of the anatomy and pathophysiology of the neck is required.
- The Neck Is Composed Of:
- Seven vertebrae (bones of the neck)
- These bones come together and form joints of our neck called facet joints
- In-between these joints, nerves exit
- Our neck has deep and superficial muscles

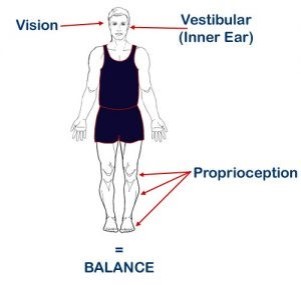
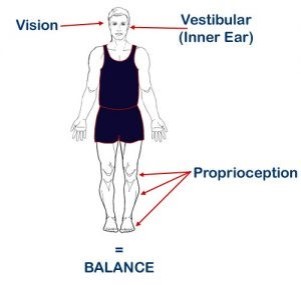
- How Does Our Neck Help Us Balance?
- Within our muscles and joints we have small sensors that send information about where our head/body is in space.
- This information travels up the neck, through our nerves and into our brain.
- These sensors are activated when our muscles stretch and shorten, or when our joints bend with movement.
- This system is called proprioception.

Possible Pathophysiology Of Cervicogenic Dizziness
- It is believed that injury to the neck may interfere with the balance system by damaging muscles, joints, or nerves that send proprioception information to the brain.
- Proprioception is one of many systems that help us maintain balance.
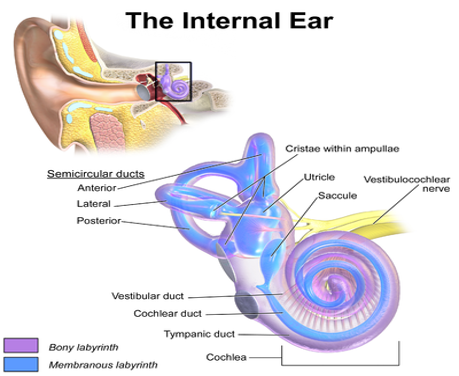
- Our brain uses multiple systems/senses to help us balance:
- Vision
- Touch
- Vestibular (inner ears)
- Proprioception
- All of these systems must come together in a process called “sensory integration” for us to balance properly.
- If one system, such a proprioception, is sending inaccurate information or contradicts the information from other systems, this can trigger dizziness.
- It is important to note that currently the pathophysiology of CD is theoretical and mostly based off of animal studies.
What Are Common Causes Of Cervicogenic Dizziness?
Mechanical forces that cause inflammation or irritation of nerves, muscles, or facet joints in our neck, which may cause altered proprioception signals.
- Common Causes:
- Chronic neck pain: creating general neck stiffness and muscle tension
- Whiplash Associated Disorders (WAD)
- Concussion
- Gate Control Theory of Chronic Pain: Before they can reach the brain, pain messages encounter “nerve gates” in the spinal cord that open or close depending upon a number of factors (possibly including instructions coming down from the brain). When the gates open, pain messages “get through” more or less easily and pain can be intense. When the gates close, pain messages are prevented from reaching the brain and may not even be experienced. Pain messages may be overridden/modulated by other signals/inputs such as massage, heat, cold, TNS (transcutaneous nerve stimulation), acupuncture, etc. (Information from: www.spine-health.com/conditions/chronic-pain/gate-control-theory-chronic-pain).
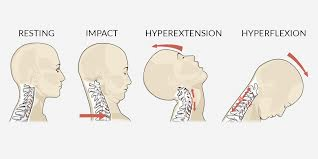
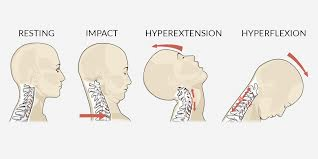
- Whiplash: Neck injury due to forceful, rapid back-and-forth movement of the neck
- This “whiplash” motion occurs during motor vehicles accidents, unexpected falls, or any direct blow to the head.
- The quick “whip” like motion of the neck can cause muscle and joint damage.
- Common symptoms of Whiplash Associated Disorders (WAD):
- Neck pain, stiffness, muscle guarding, tension
- Abnormal posture and movements: moving “on block” or very rigid
- Dizziness and instability
- Dizziness correlates with high levels of neck pain
- Only a small portion of patients suffering from WAD will experience dizziness
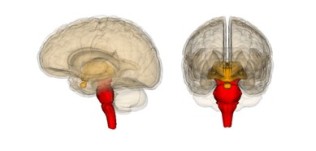
- Concussion/Traumatic Brain Injury (TBI): An injury to the brain that results in temporary loss of normal brain function.
- There are two different mechanisms for sustaining a concussion:
- Coup: Occurs at the location of the initial impact
- Counter Coup: Occurs opposite of the initial impact due to momentum pushing the brain into the skull
- Concussion may be caused by rapid head movement (without any direct hit/impact).
- Head injuries may have concomitant neck injuries due to the high forces of the direct blow causing joint and muscle damage.
- Often times prolonged concussion symptoms may be caused by undiagnosed neck dysfunction, including WAD and CD.


Symptoms Of Cervicogenic Dizziness
- Whiplash and Concussion/Traumatic Brain Injury may cause “sensory integration” problems resulting in vestibular symptoms such as:
- Dizziness
- Imbalance
- Headache/Migraine
- Vision Problems
- Brain Fog
- The onset of vestibular symptoms may be delayed 1-2 weeks after injury.
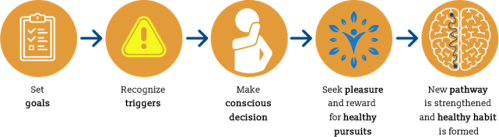
How Physical Therapy Can Help
- Head and neck injuries as well as sensory integration problems may be improved with physical therapy exercises.
- Usual recovery with physical therapy is about 3-6 weeks (for about 50% of patients).
- If regular activity is resumed too quickly prior to fully recovering from injury and sensory integration problems, the patient may decompensate and experience a relapse of symptoms.

More Information About Cervicogenic Dizziness
Cervicogenic Dizziness Article from the Vestibular Disorders Association

Kaela Pauly, DPT
of Cascade Dizziness & Balance PT
Kaela has a Doctorate in Physical Therapy (DPT) from the University of Colorado. While in school, Kaela developed a strong interest in vestibular rehabilitation when she completed a clinical rotation in an outpatient neurologic clinic. Since that time, she has continued to evolve in her expertise in this area through coursework, mentorship and self-study.
With a natural sense of adventure, Kaela has worked as a traveling physical therapist in remote areas such as Alaska, rural Colorado and towns throughout the Pacific Northwest. Those opportunities provided her with invaluable experience in outpatient, inpatient and home health settings and she was able to see how balance and vestibular disorders effect people of all ages and backgrounds.
“I love working with balance and vestibular disorders because every patient is different in how they present and each require their own unique treatment.”
*******
Presentation information is not meant to be taken as medical advice.
Presentations posted online may include discussion notes, links, images, and other information added by Seattle Dizzy Group.
*******
© Copyright 2019, Seattle Dizzy Group. All rights reserved.



























 2018 Highlights
2018 Highlights





















You must be logged in to post a comment.